Case Study: Multiple Lapses Result in Patient Fall and Injury
Case Details
A male in his mid-sixties presented to his local emergency department (ED) with complaints of shortness of breath and chest pain. He had a history of chronic obstructive pulmonary disease (COPD) and cardiovascular disease (CVD). The patient was admitted to the hospital for exacerbation of COPD symptoms and atypical chest pain.
At various times, the patient was noted to be a fall risk, and he fell twice while in the acute care area of the hospital. After the patient was transferred to the hospital’s rehabilitation unit, he was found on the floor and diagnosed with a fractured hip. The patient stated that he tried to contact a nurse for help to the bathroom, but no one responded. The patient’s wife alleged that he was overmedicated with acetaminophen/hydrocodone and zolpidem, which increased his risk of falling.
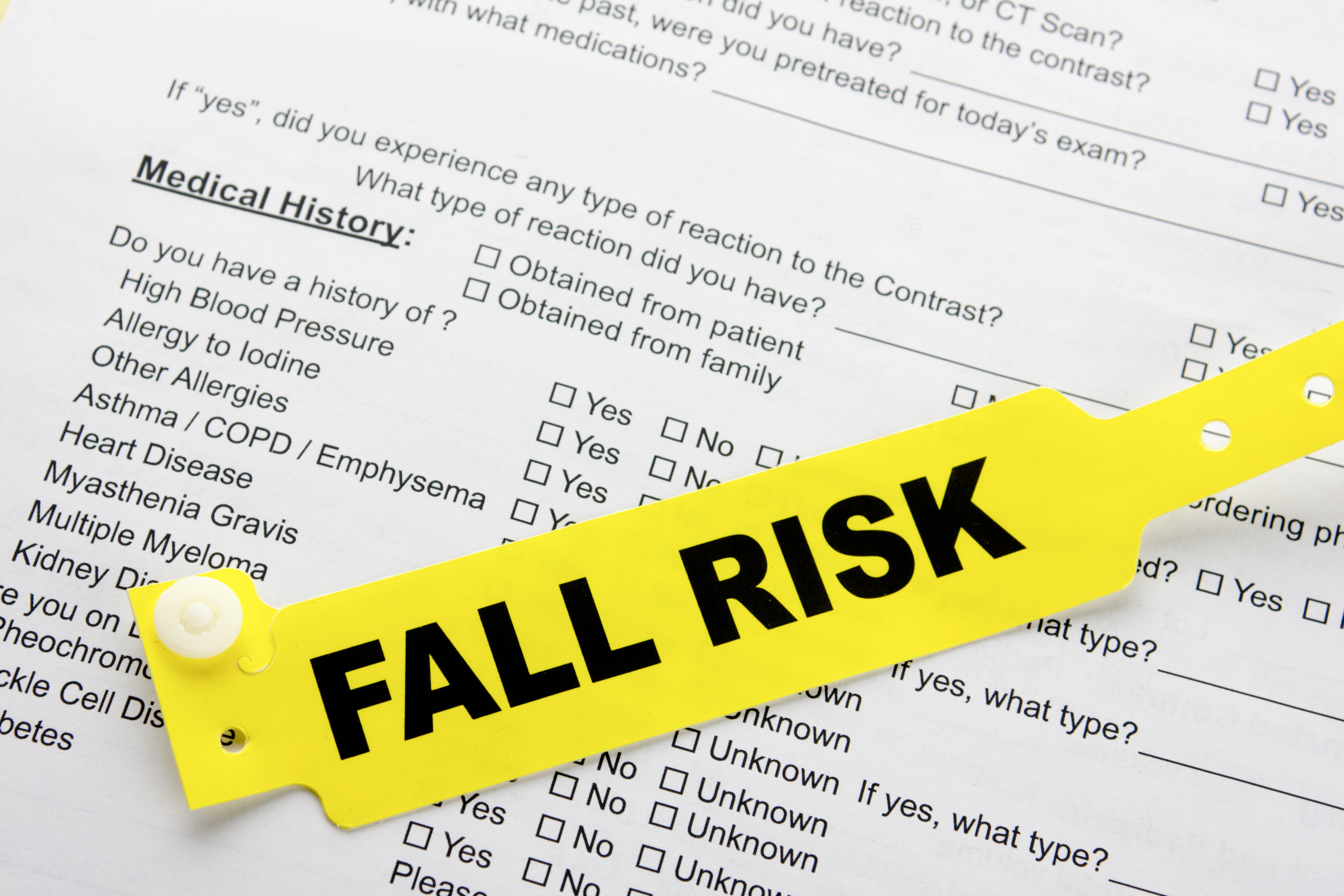
No visible reminders were in place to alert staff that the patient was a fall risk (e.g., signage or a wristband). An order stipulated that the patient should receive zolpidem at 1900. The nurse documented that zolpidem was administered at 1930; however, the hospital pharmacy software automatically assigned 2100 on the medication sheet because hospital policy stipulated that zolpidem should be administered at 2100, and any deviation required pharmacy approval. The nurse claimed that she had checked on the patient 15 minutes prior to his fall and he was sleeping.
Ultimately, the patient underwent surgical hip repair. After additional rehabilitation, the patient was discharged and returned home. However, he died 2 weeks later. A malpractice suit was filed alleging improper management of the patient’s medication regimen and failure to monitor the patient’s physiological status.
During litigation, the patient’s primary care physician testified that he spoke to the patient the morning after he fell. At that time, the patient told the physician that he used the call light to request assistance getting to the bathroom, but nobody responded. As a result, the patient attempted to get out of bed on his own and got caught in cords and wires that were attached to him, causing him to fall. Further, during testimony, a nursing expert noted several additional safety issues, including no bedside commode, bed alarm, signage on the door, or sitter to watch the patient.
Risk Management Issues
- Electronic health record discrepancies. The hospital software automatically logged the administration of zolpidem at 2100, rather than the time it was actually administered. This automatic override resulted in inaccurate documentation of patient care.
- Clinical environment issues. Various nurses and nursing assistants claimed that the unit where the patient was placed was chronically shorthanded, and staff members often were pulled to other units. Further, the nurses on the unit were distracted that evening by another patient who was insistent on getting out of bed. The patient’s nurse claimed that she alerted the charge nurse that evening that more help was needed. However, the charge nurse denied that conversation. Additionally, the patient told his primary care physician that he fell because he got caught in wires and cords attached to him, raising the question about whether proper protocols were in place to ensure environmental safety.
- Inconsistent documentation. The patient’s primary care physician testified that when he spoke to the patient about the fall, the patient did not complain of feeling woozy or overmedicated; however, the nurse had documented that the patient felt woozy at the time the zolpidem was administered.
- Administrative lapses. The original order for zolpidem stipulated it should be administered at 1900, but actual administration occurred at 1930. The hospital had a policy that required pharmacy approval for any deviation from administering zolpidem at 2100; the approval was not obtained in this case. Additionally, despite the patient being a known fall risk, proper precautions were not in place to alert providers/staff (e.g., signage or a wristband) and attempt to reduce the patient’s risk of falling (e.g., timely response to the call light or availability/use of a bedside commode, bed alarm, or sitter).