Assessing Diagnosis-Related Allegations in Otolaryngology Claims: The Complexities of Clinical Reasoning
Laura M. Cascella, MA, CPHRM
Diagnostic errors are a persistent issue in healthcare, and they are top liability risk for many medical specialties. A review of 10 years of closed claims data for otolaryngology shows that diagnosis-related allegations account for almost 1 in 5 claims.1
Although the volume of diagnosis-related claims is significantly lower than the volume of claims for the top allegation category — procedural performance, which accounts for almost half of all otolaryngology claims — these cases still can be consequential in terms of poor patient outcomes and total dollars paid (i.e., expense and indemnity dollars).
Diagnosis-related otolaryngology claims often involve oropharyngeal cancers, and most of the allegations are related to a failure to order or delay in ordering diagnostic testing, which is compounded by:
- A narrow diagnostic focus, especially when faced with an atypical presentation or symptoms matching a chronic, previously known condition
- Misinterpretation of diagnostic studies
- Failure to pursue an abnormal finding
A common contributing factor in diagnosis-related claims for all specialties is clinical judgment, which includes clinical reasoning and decision-making. In otolaryngology, clinical judgment is noted as a risk factor in almost every diagnosis-related allegation.
Because clinical judgment is a complex process that involves various cognitive functions, it’s easy to understand why it is a driving force in diagnosis-related claims. Much of the literature focusing on diagnostic errors and clinical reasoning recognizes the dual decision-making model, which consists of two reasoning systems as the basis for clinicians’ diagnostic process. In System 1, the reasoning process is automatic, intuitive, reflexive, and nonanalytic. The clinician arranges patient data into a pattern and arrives at a working diagnosis based on past experience, knowledge, and/or intuition. In System 2, the reasoning process is analytic, slow, reflective, and deliberate. This type of thinking often is associated with cases that are complex or novel, and System 2 thinking involves more cognitive workload and resources.2
System 1 and System 2 are not mutually exclusive, and clinicians tend to use both, depending on the circumstances. Although research suggests that most clinical work involves System 1 reasoning — particularly as clinicians gain more experience and knowledge — both systems of reasoning are vulnerable to cognitive errors.3
Research about the cognitive aspect of diagnostic errors suggests that errors in clinical reasoning often arise from several sources, including faulty heuristics, cognitive biases, and affective influences.4
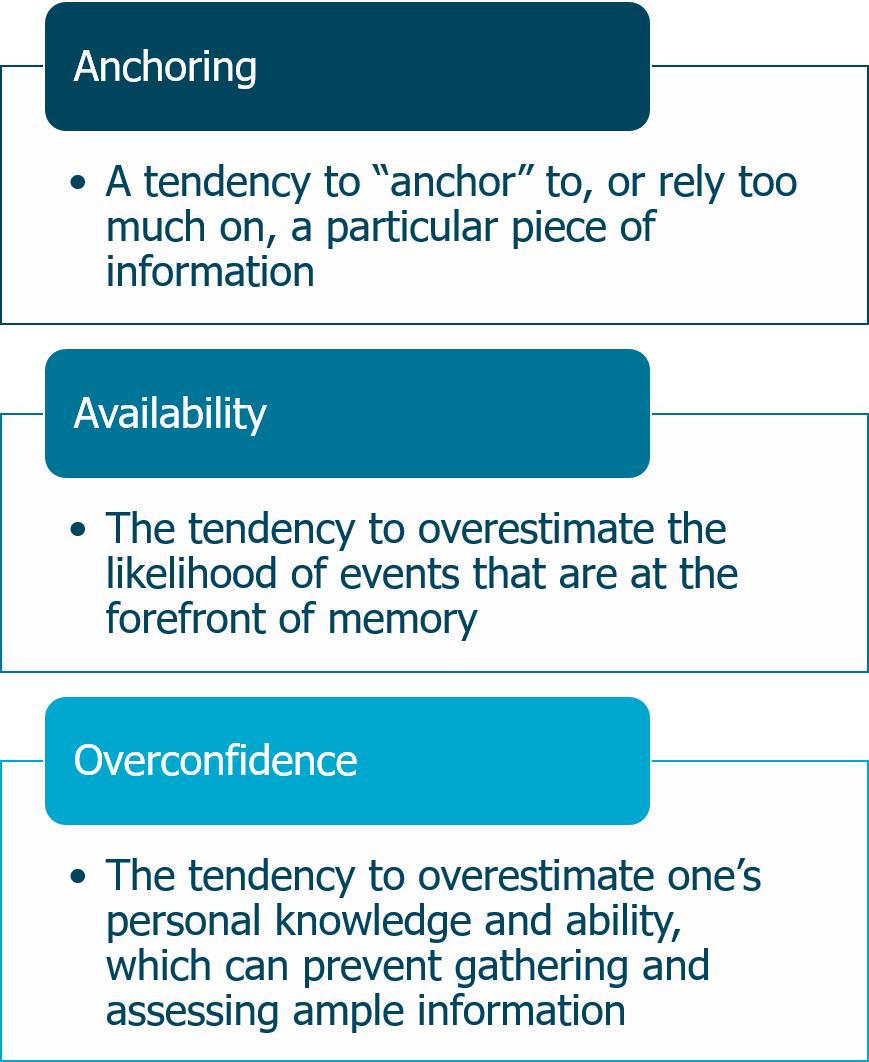
The term “heuristics” refers to mental shortcuts in the thought process that help conserve time and effort. These shortcuts are an essential part of thinking, but they are also prone to error. Cognitive biases occur when heuristics lead to faulty decision-making. Some common biases included anchoring, availability, and overconfidence.
The term “affective influences” refers to emotions and feelings that can sway clinical reasoning and decision-making.5 For example, preconceived notions and stereotypes about a patient might influence how the practitioner views the patient’s complaints and symptoms.
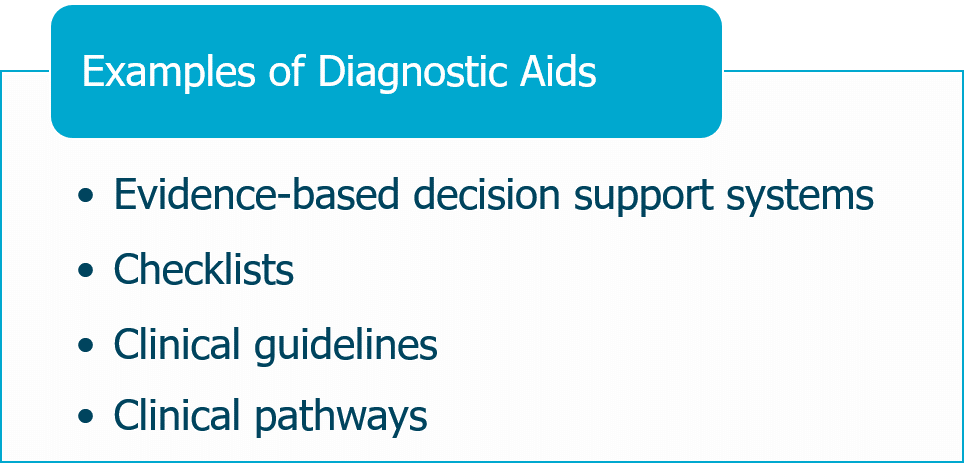
Although cognitive processes are well-studied, further research is needed to determine how best to prevent the flaws in clinical judgment that can lead to diagnostic errors. A number of potential solutions have been proposed, including implementing strategies to improve teamwork, adjusting processes and workflows, using diagnostic aids, and exploring debiasing techniques. Yet, researchers note that “unless [these strategies] are well integrated in the workflow, they tend to be underused.”6
Thus, carefully considering how various diagnostic strategies can be implemented in everyday clinical activities may help otolaryngologists begin to take steps toward managing diagnostic risks. A helpful resource is the Society to Improve Diagnosis in Medicine’s Clinical Reasoning Toolkit for trainees, clinicians, and educators. The toolkit supports awareness and better understanding of diagnostic reasoning, cognitive psychology, and diagnostic errors. Resources within the toolkit include links to books and articles, slide presentations, and videos focusing on clinical reasoning and cognitive errors.
Endnotes
1 MedPro Group. (2020). Otolaryngology: Claims data snapshot. Retrieved from www.medpro.com/documents/10502/5086243/Otolaryngology.pdf
2 National Academies of Sciences, Engineering, and Medicine. (2015). Improving diagnosis in health care. Washington, DC: The National Academies Press; Nendaz, M., & Perrier, A. (2012, October). Diagnostic errors and flaws in clinical reasoning: Mechanisms and prevention in practice. Swiss Medical Weekly, 142, w13706; Phua, D. H., & Tan, N. C. (2013). Cognitive aspect of diagnostic errors. Annals of the Academy of Medicine, Singapore, 42(1), 33–41; Ely, J. W., Graber, M. L., & Crosskerry, P. (2011, March). Checklists to reduce diagnostic errors. Academic Medicine, 86(3), 307–313.
3 Phua, et al. Cognitive aspect of diagnostic errors; Nendaz, et al., Diagnostic errors and flaws in clinical reasoning; Crosskerry, P., Singhal, G., & Mamede, S. (2013, October). Cognitive debiasing 1: Origins of bias and theory of debiasing. BMJ Quality & Safety, 22(Suppl 2), ii58–ii64.
4 Phua, et al. Cognitive aspect of diagnostic errors.
5 National Academies of Science, Engineering, and Medicine, Improving diagnosis in health care; Crosskerry, P., Abbass, A. A., & Wu, A. W. (2008, October). How doctors feel: Affective influences in patient’s safety. Lancet, 372, 1205–1206; Phua, et al. Cognitive aspect of diagnostic errors.
6 Ely, et al., Checklists to reduce diagnostic errors.