15 Strategies for Tackling the Top Malpractice Allegation in Gynecology
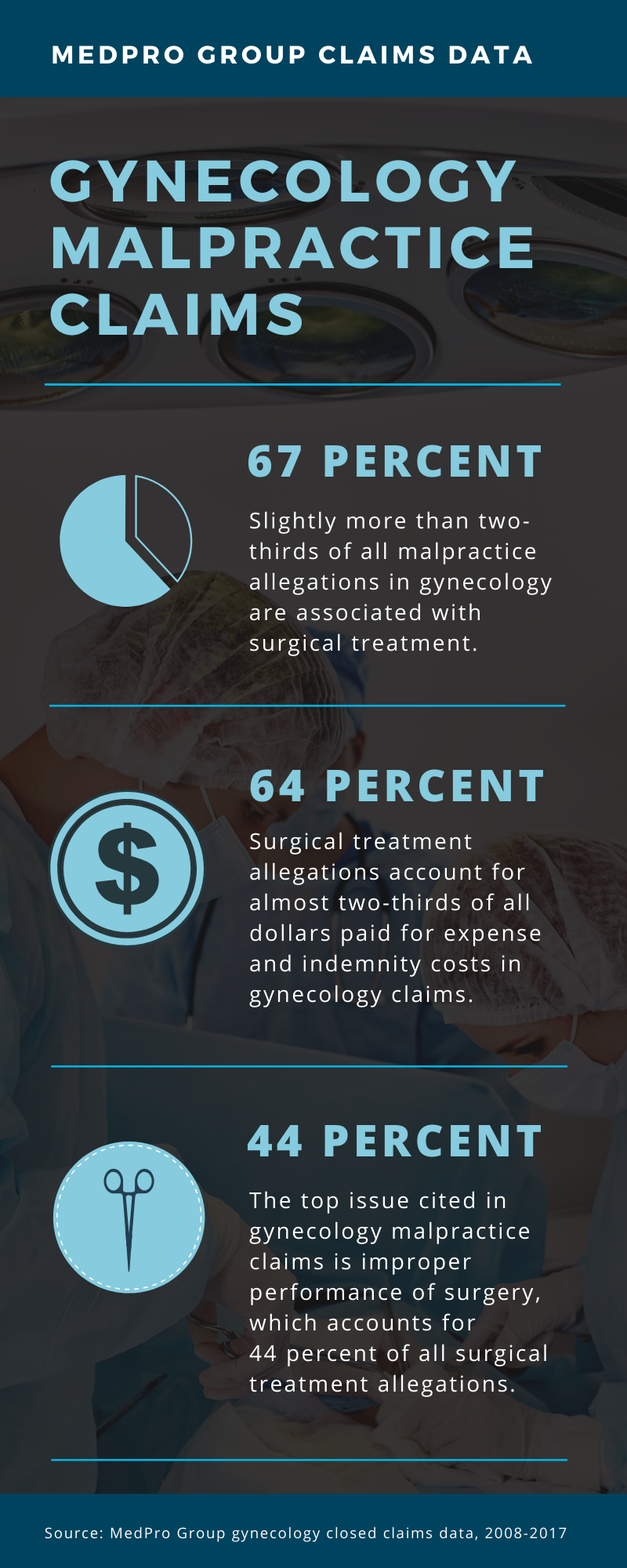
MedPro Group data show that allegations related to surgical treatment represent the largest claims category for gynecology providers (67 percent of all gynecology claims closed between 2008 and 2017). Surgical treatment allegations also account for almost two-thirds of all dollars paid for expense and indemnity costs associated with gynecology claims.
Within these surgical treatment allegations, the top issue cited is improper performance of surgery, which accounts for 44 percent of surgical treatment claims. These allegations most often are the result of a known complication of a procedure (e.g., a bowel or bladder laceration); however, these situations often are complicated by a failure to recognize and act upon patients’ changing postoperative clinical conditions.
Other issues cited include improper management of surgical patients and retained foreign bodies. Improper management includes various suboptimal situations during the perioperative period, such as inadequate monitoring of vital signs, improper surgical skin site preparation, and delayed recognition of complications following discharge. Although relatively few claims are associated with retained foreign bodies, these allegations are still a concern, and most often they are noted in abdominal hysterectomy cases.
The following list offers strategies to help healthcare organizations and gynecology providers manage surgical treatment risks:
- Adhere to well-defined credentialing, recredentialing, and privileging policies that incorporate ongoing practice performance evaluation and focused professional practice evaluation. Credentialing and privileging should include evaluation of surgical skills and competency with surgical equipment.
- Implement peer review processes and conduct peer review activities to improve performance and quality. Routinely evaluate quality indicators and implement performance improvement plans to address safety risks and improve quality of care.
- Engage in ongoing continuing medical education and training opportunities to enhance technical surgical skills and communication skills.
- Conduct thorough informed consent discussions with patients, including a review of risks, benefits, and alternative treatments. Speak in layman’s terms during these discussions, and use a technique such as teach-back to gauge patients’ comprehension of information.
- Document informed consent discussions, including the provision of verbal and written patient education; make sure any signed informed consent forms are included in patients’ records.
- Verify that each patient’s record contains thorough and appropriate information, such as history and physical, current medications, nonpharmacological interventions, allergies, pain assessment outcomes, test results, consults/referrals, treatment goals, and preoperative screening results.
- Conduct a thorough preoperative screening of each patient for risk factors, and ensure that all appropriate health information for the patient is available prior to commencement of a procedure.
- Inventory and verify necessary equipment and supplies before each procedure begins.
- Ensure infection prevention and control best practices (e.g., those related to hand hygiene, safe injections, skin preparation, instrument sterilization, environmental cleaning, etc.) are used to maintain the sterile field.
- Use standardized patient safety precautions during each procedure, such as timeout protocols, proper patient positioning, surgical item counts, etc.
- Make sure patients are appropriately monitored during and following procedures (e.g., vital signs, airway, and pain).
- Maintain a consistent postoperative discharge assessment process, and carefully consider repeated patient complaints or concerns when making clinical decisions about patient care and diagnostic testing.
- Provide patients and caregivers with written and verbal instructions related to their treatment plans and follow-up care.
- Complete a detailed operative report on the day of each procedure.
- Document all instances of patient nonadherence as they occur using objective information, and document any follow-up education provided to the patient or caregiver to address nonadherence.