Data Insight: The Role of Documentation in Inpatient Surgical Treatment Malpractice Claims
Accurate, clear, and timely documentation of the clinical progression of patients is critically important in both acute and ambulatory care. Yet, documentation continues to represent an area of risk.
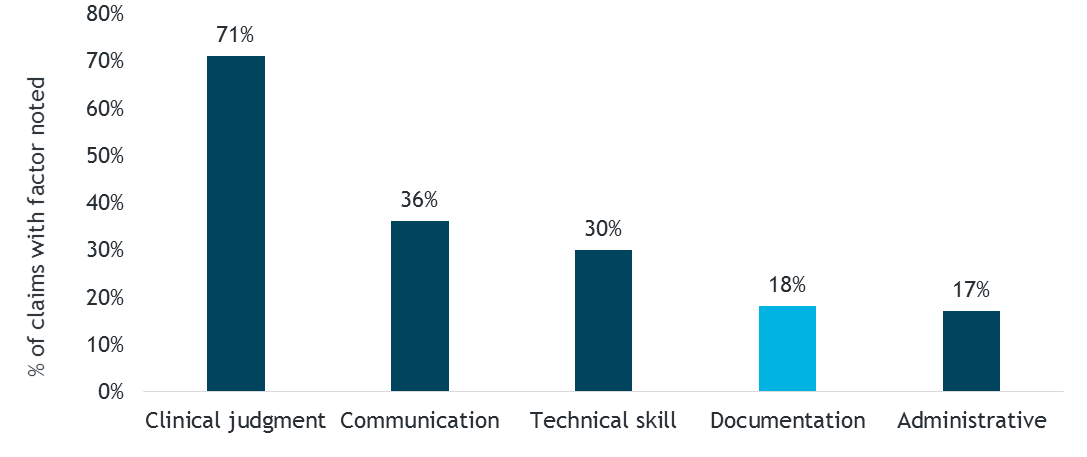
An analysis of 10 years of MedPro closed claims history shows that documentation issues consistently are in the top five risk factors associated with inpatient claims that have clinically severe outcomes (i.e., permanent disability or death).
Figure 1. Risk Factors in High-Severity Inpatient Claims
Claims involving documentation issues also tend to involve more expensive resolutions in terms of total dollars paid for expense and indemnity costs. Thus, both clinical and financial severity in inpatient malpractice claims point to the importance of reviewing documentation protocols as part of risk management efforts.
Considering that the health record serves as a primary source of information as inpatient care transitions from provider to provider, insufficient or incorrect documentation of clinical information, date/time of treatment, and even a provider’s clinical rationale for a course of treatment can have profound effects on the process of care for patients and the risk of liability for healthcare providers and organizations.
Documentation as a Malpractice Risk Factor
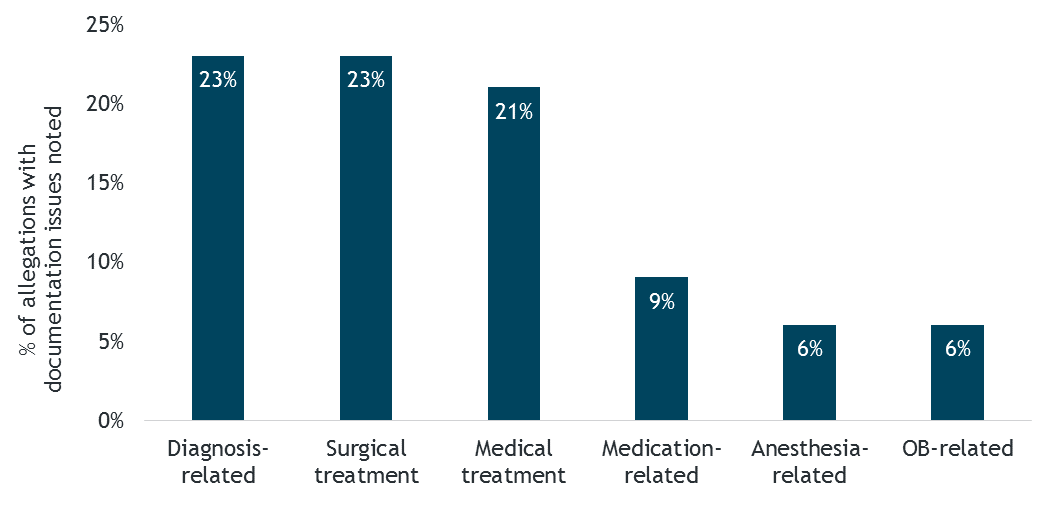
Across inpatient and outpatient allegations, documentation missteps are most frequently noted in diagnostic, surgical, and medical treatment allegations — and these categories are fairly balanced, as shown in Figure 2.
Figure 2. Top Allegation Categories for Documentation Issues
However, when examining the inpatient claims only, surgical allegations quickly rise to the top — 75 percent of inpatient claims involving documentation issues arise from a surgical encounter. The documentation issues noted in these claims may occur during surgery or during the postoperative management of a patient.
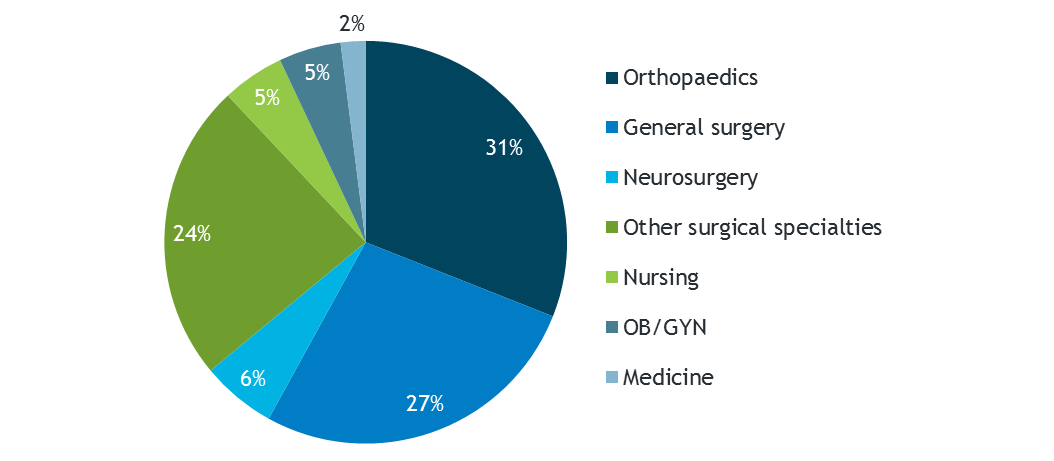
A closer look at high-severity surgical treatment allegations involving documentation issues shows that orthopaedic and general surgery procedures account for more than half of the total claim volume (see Figure 3).
Figure 3. High-Severity Surgical Treatment Allegations Involving Documentation Issues, by Specialty
Further, high-severity surgical treatment claims involving documentation issues are more costly than those that do not involve documentation issues — total dollars paid per claim is 42 percent higher.
Generally, insufficient/incorrect documentation does not directly cause poor surgical outcomes; however, lapses in documenting operative reports, correct surgical counts, patient vital signs, or critical lab results can lead to suboptimal patient outcomes and make subsequent malpractice cases more difficult to defend. Scenarios showcasing the impact of insufficient/incorrect documentation in a surgery setting include:
- Failure to dictate an operative report followed by an emergent need to return the patient to surgery with no documentation of the clinical findings from the first surgery
- Failure to consistently record patient vital signs, especially in surgeries involving massive blood loss
Details and Case Studies
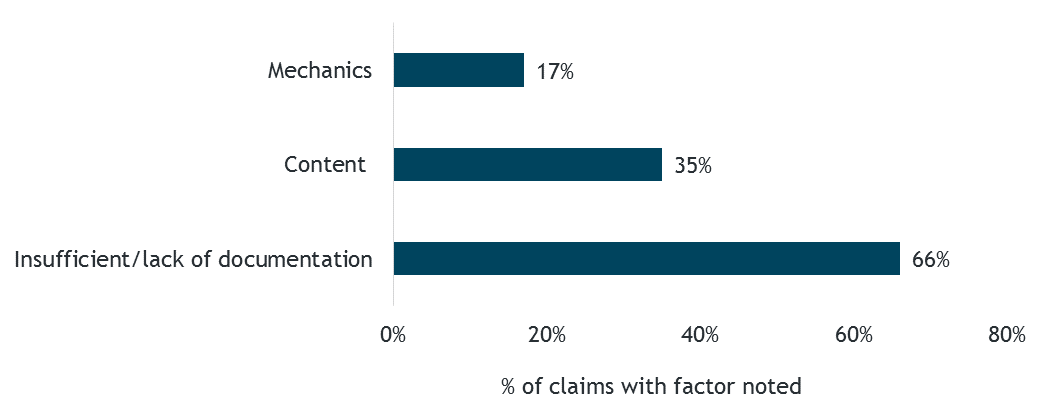
A critical risk management focus is addressing insufficient documentation of clinically important information in medical records. This issue is noted in two-thirds of high-severity surgical treatment claims involving documentation, followed by content factors (inconsistent documentation among caregivers or altered information) and the actual mechanics of documenting (illegibility issues in paper charts, incorrect or inaccurately transcribed orders, etc.).
Figure 4. Type of Documentation Issues in High-Severity Inpatient Surgical Treatment Claims
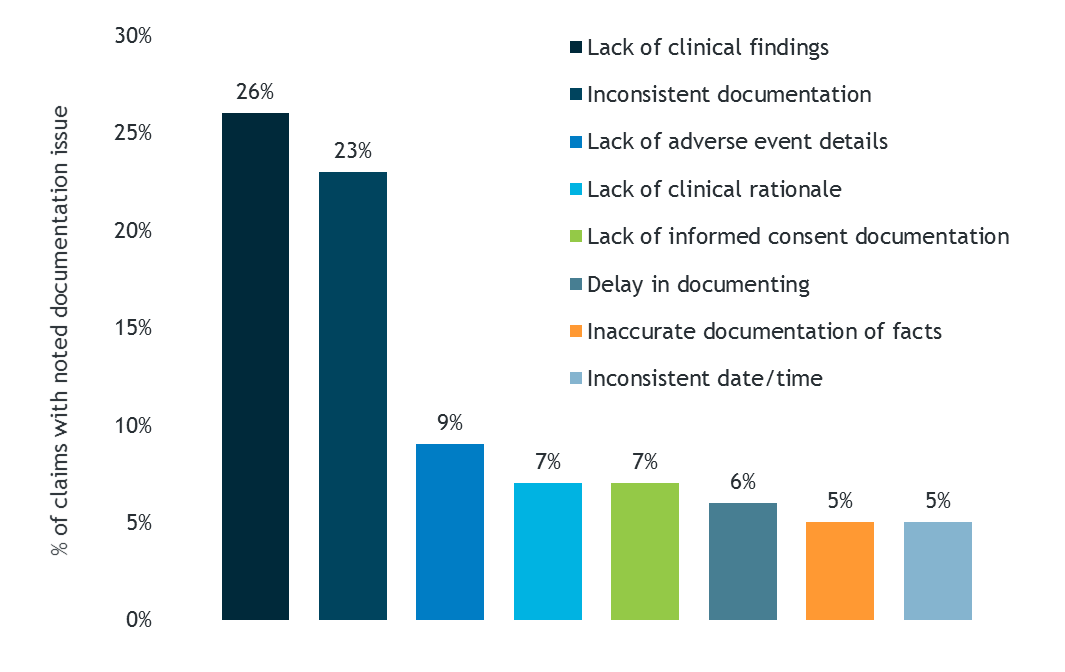
The details of these documentation risk factors are shown in Figure 5; this information can be used to hone quality audits and risk mitigation strategies in a hospital/facility setting.
Figure 5. Breakdown of Types of Documentation Issues in High-Severity Inpatient Surgical Treatment Claims
Case Scenario One
A patient in his early sixties presented for surgical repair of acute appendicitis. A surgical resident documented the patient’s medical history, including repair of a hernia with placement of mesh. The surgeon did not read the health record prior to surgery, and therefore did not adjust his surgical technique to avoid puncturing the area of mesh. An unrecognized bowel perforation also occurred during the surgery. The dictated operative report did not include documentation of the surgeon’s complete visualization of the operative site.
Postoperatively, the patient developed significant abdominal pain and distension. A CT scan was ordered, which revealed free air in the abdomen. Unfortunately, the surgeon did not review the report for 8 hours after it was available in the health record. The patient was returned to surgery to repair the perforation, but he experienced complications over the next month including peritonitis, septic shock, and respiratory failure.
Case Scenario Two
A patient in her early fifties presented for a total hip replacement due to severe degenerative arthritis. Postoperative documentation indicates that the surgery site was examined prior to final closure and no complications were noted. In recovery, the nurse noted that the patient was able to move her toes, but the nurse did not document pedal pulse assessments.
After the patient was transferred to the orthopaedic unit, nursing staff documented sluggish capillary refill, a cool foot, and no palpable pedal pulses. However, staff members did not document ongoing neurovascular assessments, which ultimately led to a several hour delay in diagnosing an adverse outcome.
The patient’s condition continued to deteriorate. Upon emergent return to the operating room, a complete transection of the femoral artery was discovered. Postoperatively, the patient sustained a pulmonary embolus and developed compartment syndrome. She was left with no mobility in her ankle and foot due to nonfunctioning nerves in her leg.
Key Points
- Contemporaneous, complete, and consistent documentation is an extremely important part of the surgical process, and it is also critical to the successful defense of potential malpractice claims.
- Failure to follow an organizational protocol for performing and documenting routine postoperative vital sign checks can have devastating consequences; generally, the assumption is that “if it wasn’t documented, it wasn’t done.” The same is true of failure to document the date/time that critical test results are received and communicated.
- Effective communication among healthcare providers often is dependent on accurate and timely documentation. In fact, communication-related risk factors are concurrently noted across half of high-severity inpatient surgical treatment allegations. Improving documentation processes can support high-quality patient care; however, remember that good documentation is useless if not available, read, and acted on.
Resources
Data Source
MedPro Group closed claims data, 2007–2016